When you click on links to various merchants on this site and make a purchase, this can result in this site earning a commission. Affiliate programs and affiliations include, but are not limited to, the eBay Partner Network.
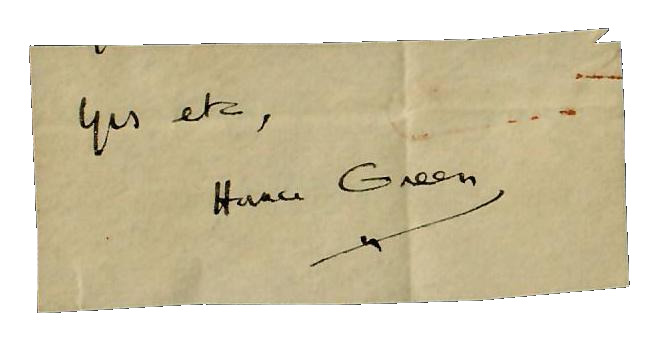
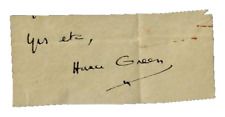
Up for sale a RARE! "Father of Laryngology" Horace Green 1.25X3 Clipped Signature. This is the only signature to come to sale in more than 30 years as most are in museums and university collections.
ES-7727E
Horace Green
(1802-1866) (figure 1) was the first specialized airway physician in the United
States and endures as one of the greatest pioneers in American medical history.
His life's work was committed to diseases of the pharynx, larynx, and trachea,
which are key missions of the American Broncho-Esophagological Association. The
founder of our society, Chevalier Jackson (1865-1958), was interested in
similar subject matter, which is keenly illustrated by the authors' writing and
research. [1-15] Additionally, both physicians were strong advocates of education.
[16, 17] Among Green's monumental seminal contributions are that he was the
first individual; 1. to directly treat diseased mucosa of the tracheo-bronchial
tree [1], 2. to perform direct laryngoscopy and 3. to endoscopically resect a laryngeal
lesion with the visual control. Horace Green was born in Chittenden, Vermont on
December 24, 1802. Green's grandfather was a Massachusetts physician, who had
four sons that fought in the American Revolution. Green's father was the only
son who survived while his three brothers all died in combat. Green was the
youngest of four sons and graduated from Castleton Medical College in 1824. In
1830, he attended further lectures at the University of Pennsylvania. After
practicing for a few years in Vermont, Green moved to New York City in 1835. He
traveled to Europe in 1838 to advance his studies and initiated his
investigations in throat diseases upon returning to New York, where he
practiced most of his career. Descriptions of infectious diseases of the airway
date back thousands of years. There have been a wide variety of names including
phthisis, cynanche laryngeal, quinsy, laryngeal and pharyngeal angina,
diphtheria, tuberculosis, consumption, and croup. From ancient civilizations
through the 19th century, tracheotomy, a primary treatment, was seldom done due
to skepticism and limited understanding of human physiology and the biology of
these diseases. However, in the earlier 1800s, there was a substantial
expansion of investigations and reporting on these diseases. Bretonneau
(1778-1862) [18, 19], Ryland (1806-1857) [20], Trousseau (1801-1867) [21-23],
and Green [1-5, 7] led this effort. All were focused on surgical intervention
of the larynx and trachea to avert the moroffer and frequently fatal
complications of these diseases, however, Green was substantially more focused
on transoral instrumentation with topical administration of caustics to the
diseased laryngo-tracheal mucous membranes. Possibly the earliest description of endolaryngeal intubation
was by Avicenna (980-1037), who bent tubes of gold and silver to cannulate the
larynx and trachea for patients with airway distress. In the late 18th century,
Desault (1744-1795) [24-27], who was the Surgeon in Chief of the Great Hospital
of the Humanity in Paris revived intubation and described passing a
nasotracheal tube to secure the airway. He also was skilled in open
transcervical operative techniques and is probably the first surgeon to stress
the importance of surgeons retaining skill-sets in transoral and open surgical
methods. Desault's technique was well known at the time and described in the
famous surgical text by Malgaigne (1806-1865). [26, 27] A century later, this
philosophy was more firmly established by Solis Cohen who was probably the
first surgeon to specialize as a Laryngologist. There was a substantial need
and interest for novel transoral management of infectious airway diseases in
Green's era was due to potentially lethal consequences of these disorders as
well as the procedure of tracheotomy. However, the emotions of patient's and
clinicians were not surprisingly reflective of the severity of the problem and
the frustration of inconsistent treatment outcomes. Despite the expanding acceptance and
performance of tracheotomy in the 19th century, the procedure continued to be
appropriately perceived by most clinicians as a heroic intervention to be done
in dire circumstances often when the patient was already in extremis. This was
especially so for those attempting tracheotomy in children. Billroth
(1829-1894), who successfully performed the first total laryngectomy for cancer
[29], provides a compelling description of tracheotomy in a six year-old child.
This individual was one of 12 laryngotomy/tracheotomy procedures that he
reported for treating croup in children. ìThis is the only case in which a
patient has ever died immediately under the knife at my hands. It made a great
and permanent impression on my mind, and has been to me a most decided warning
against ever attempting tracheotomy again when single-handed. Intraprocedural
bleeding was commonplace during tracheotomy due to the thyroid gland and
anterior jugular veins. If excessive blood was aspirated into the trachea
and/or the patient was exhausted and unable to expectorate ominous
circumstances ensued. The surgeon would frequently be required to place a
catheter into the airway and clear the trachea by personally suctioning the
blood and purulence with his/her own mouth. [23, 27, 30, 31] Even today,
thoracic surgeons will similarly pass a flexible bronchoscope to aspirate blood
and debris on surgical patients. The majority of patients who underwent
tracheotomy died despite the airway procedure because the underlying systemic
disease process had not been reversed. As to be expected, most aspects of this
management were considerably more problematic in children. Indwelling tubes
were not yet perfected and often became occluded and/or dislodged. Adequate
lighting was frequently lacking and suction was not yet unavailable. In fact,
casts of blood, and mucopurulent sloughing membrane had to be removed manually
from the trachea by removing the tube. Regardless of whether surgeons
adopted a transoral/transnasal approach or tracheotomy to remedy airway
obstruction, infectious membranous airway maladies created a medical and
surgical imperative to access/treat the diseased mucosa. Profound medical or
surgical needs typically catalyze paradigm-changing interventions. [33] Topical
pharmacological agents such as silver nitrate or mercurial compounds were
mainstays of treatment in the 19th century and the aforementioned airway
interventions also provided a route of administration for delivering these agents.
However, these topical agents did not treat the underlying disorder, which is
why mortality rates remained high despite frequent successful airway
palliation. Despite a range of systemic pharmacological treatment strategies
leading to successful management of most infectious airway ailments in the 20th
century, aggressive recurrent respiratory papillomatosis remains as a the
21st-century vestige of this era since systemic control remains disappointing.
Possibly the earliest description of endolaryngeal intubation was by Avicenna
(980-1037), who bent tubes of gold and silver to cannulate the larynx and
trachea for patients with airway distress. In the late 18th century, Desault
(1744-1795) , who was the Surgeon in Chief of the Great Hospital of the
Humanity in Paris revived intubation and described passing a nasotracheal tube
to secure the airway. He also was skilled in open transcervical operative
techniques and is probably the first surgeon to stress the importance of
surgeons retaining skill-sets in transoral and open surgical methods. Desault's
technique was well known at the time and described in the famous surgical text
by Malgaigne (1806-1865). [26, 27] A century later, this philosophy was more
firmly established by Solis Cohen who was probably the first surgeon to
specialize as a Laryngologist. There was a substantial need and interest for
novel transoral management of infectious airway diseases in Green's era was due
to potentially lethal consequences of these disorders as well as the procedure
of tracheotomy. However, the emotions of patient's and clinicians were not
surprisingly reflective of the severity of the problem and the frustration of
inconsistent treatment outcomes. Despite the expanding acceptance and
performance of tracheotomy in the 19th century, the procedure continued to be
appropriately perceived by most clinicians as a heroic intervention to be done
in dire circumstances often when the patient was already in extremis. This was
especially so for those attempting tracheotomy in children. Billroth
(1829-1894), who successfully performed the first total laryngectomy for cancer
[29], provides a compelling description of tracheotomy in a six year-old child.
This individual was one of 12 laryngotomy/tracheotomy procedures that he
reported for treating croup in children. ìThis is the only case in which a
patient has ever died immediately under the knife at my hands. It made a great
and permanent impression on my mind, and has been to me a most decided warning
against ever attempting tracheotomy again when single-handed. Intraprocedural
bleeding was commonplace during tracheotomy due to the thyroid gland and
anterior jugular veins. If excessive blood was aspirated into the trachea
and/or the patient was exhausted and unable to expectorate ominous
circumstances ensued. The surgeon would frequently be required to place a
catheter into the airway and clear the trachea by personally suctioning the
blood and purulence with his/her own mouth. Even today, thoracic surgeons will similarly
pass a flexible bronchoscope to aspirate blood and debris on surgical patients.
The majority of patients who underwent tracheotomy died despite the airway
procedure because the underlying systemic disease process had not been
reversed. As to be expected, most aspects of this management were considerably
more problematic in children. Indwelling tubes were not yet perfected and often
became occluded and/or dislodged. Adequate lighting was frequently lacking and
suction was not yet unavailable. In fact, casts of blood, and mucopurulent
sloughing membrane had to be removed manually from the trachea by removing the
tube.